55% increase in stroke in people in their 50s
Need a free and open discussion on the possible causes.
This is the video I have just recorded on this topic with data from England.
Hospital admissions for strokes rise by 28% since 2004 – as NHS urges the public to ‘Act FAST’
(Face, Arms, Speech, Treatment)
This is the paper from NHS England.
The number of people being admitted to hospital following a stroke has risen by 28% in the last 20 years, new NHS analysis has found.
17th November 2024
https://www.nhs.uk/conditions/stroke/symptoms/
These following notes are taken from the NHS paper and discussed in the video.
NHS England data
Stroke admissions in England in 2023/24
111,137 stroke admissions
Stroke admissions in England in 2004/05
87,069 stroke admissions
(driven in part by an ageing population and the impacts of lifestyle factors on the nation’s cardiovascular health)
Stroke admissions among people aged 50-59, 2023/24
12,533
Stroke admissions among people aged 50-59, 2004/05
8,063
That is a 55% rise in admissions among people aged 50-59
Stroke admissions among people aged 60-69
42% increase
Stroke admissions among people aged 70-79
25% increase
NHS launched a major campaign
999 immediately
Struggling to smile (Face)
Raise an arm (Arms)
Slurring their words (Speech)
England’s top doctor
figures show that strokes “are not just a risk for older people”
Experts say
(increase in admissions among ages 50-59)
Better detection and reporting
Hypertension
Obesity
Poor diet
Lack of exercise
Signs Symptoms
Face weakness
Arm weakness, weakness or numbness in 1 arm
Speech problems, slur words or sound confused
Other symptoms of a stroke
Weakness or numbness down 1 side of body
Blurred vision or loss of sight in 1 or both eyes
Finding it difficult to speak or think of words
Confusion and memory loss
Feeling dizzy or falling over
A severe headache
Feeling or being sick (nausea or vomiting)
After reporting on this video I gave an introduction to the pathophysiology of stroke based on my textbook, Campbell’s Pathophysiology Notes.
Available for free download here,
https://drjohncampbell.co.uk
Cerebrovascular accident (Stroke)
Stroke is defined as a focal neurological deficit due to a vascular lesion which
lasts for more than 24 hours. Stroke is the third most common cause of death
in most developed countries, after heart disease and cancer. It is also the major
cause of disability in adults.
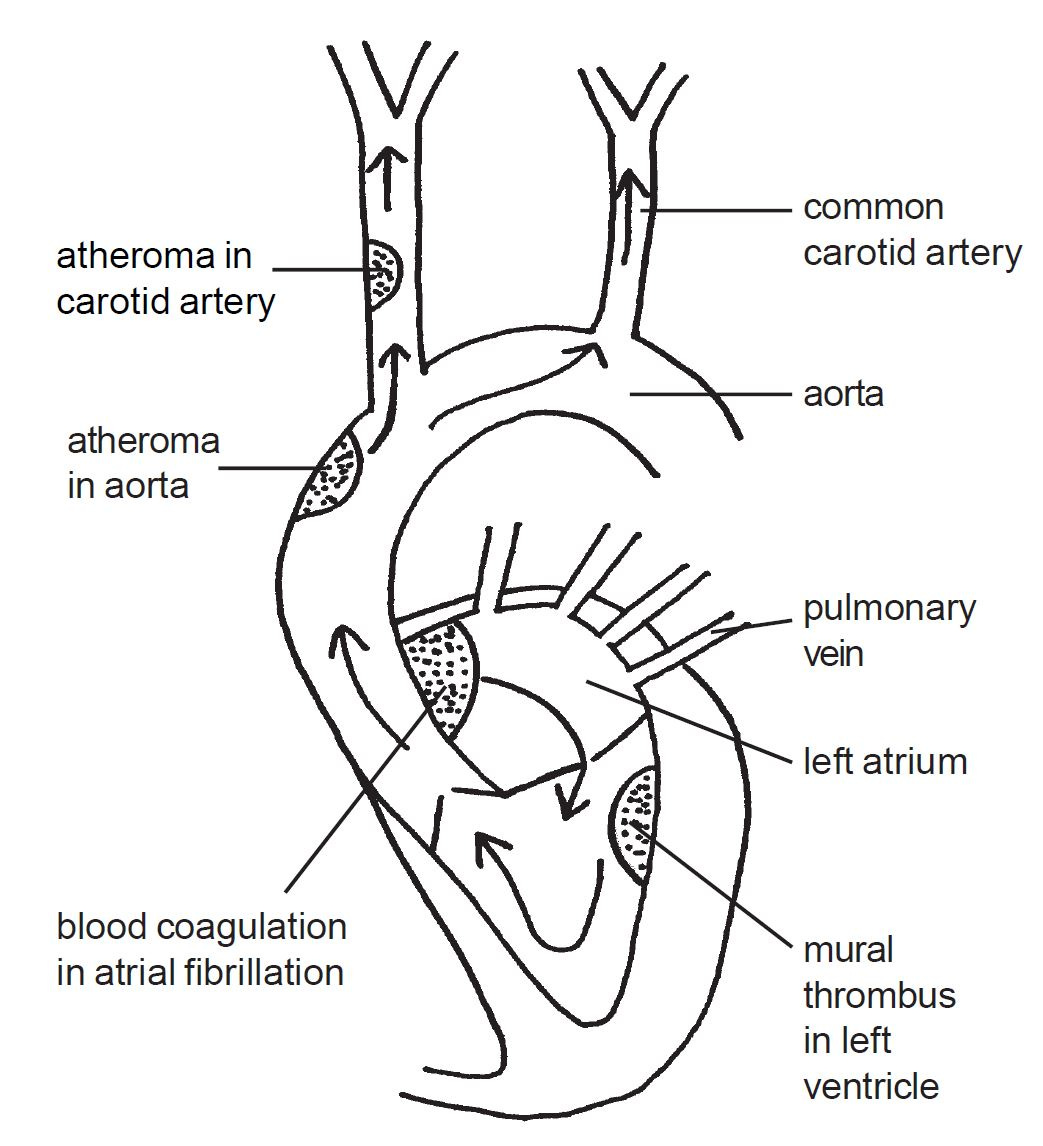
Thromboembolic pathophysiology
There are two main types of stroke; thromboembolic and haemorrhagic. As the
name implies thromboembolic stroke is caused by an occlusion of the normal
blood supply by thrombosis or embolism. This cause of stroke is most common
accounting for about 85% of cases. Thromboembolic stroke occurs mostly as a
compilation of atherosclerosis with atheroma leading to thrombus formation.
As in other forms of arterial disease a thrombus will develop on a ruptured
plaque of atheroma. The presence of a thrombus will occlude an arterial lumen
and so fully or partly cut off the blood supply to an area of the brain. Parts of
a thrombus may break away from the main clot generating emboli. When an
embolus reaches a vessel it is too large to pass through, the embolus becomes
jammed, occluding blood flow. Thromboembolic pathology may arise from
the heart and large extracranial arterial vessels supplying blood to the brain or
from smaller intracerebral vessels.
Extracranial emboli
Emboli may arise from thrombus formation in the heart. Emboli from the left
side of the heart can pass into the cerebral circulation via the aorta and account
for about 20% of thromboembolic strokes. Emboli may be generated in the
heart as a complication of atrial fibrillation, endocarditis or from a mural
thrombus which may complicate myocardial infarction.
The most common cause of stroke is emboli which arise from thrombus
development in the extracranial arteries such as the aorta, carotid or vertebral
arteries. These vessels transport blood from the left ventricle to the cerebral
arteries in the brain. The most common cerebral artery which becomes
occluded as a result of embolism is the middle cerebral artery. This artery
carries high volumes of blood from the circle of Willis to large areas of the
brain. As a result any thromboembolic occlusion of this vessel will potentially
deprive a significant area of brain of its normal blood supply resulting in a large
cerebral infarction.
Disease in intracerebral arteries
A further 20% of infarctions are due to disease within the smaller
intracerebral arterial vessels within the brain. These small penetrating arterial
branches carry blood from the larger vessels, such as the middle, posterior
or anterior cerebral arteries into the brain tissue. Disease in these smaller
vessels is most likely to develop in patients with diabetes and hypertension.
When one of these arteries becomes occluded it will infarct a small area of
the brain giving rise to a highly localised stroke. For example, the patient
may present with only loss of motor or sensory function, as opposed to
most strokes when both are lost in the same area of the body. The relatively
small lesions generated by disease of these penetrating vessels are termed
lacunar infarcts. Because they do not involve a large area of the brain they
are unlikely to cause impairment of cognition, memory, speech, or level of
consciousness. Despite only affecting relatively small areas of the brain the
effects of a small infarct can be significant, especially as they may affect the
nerve fibres within the internal capsule.
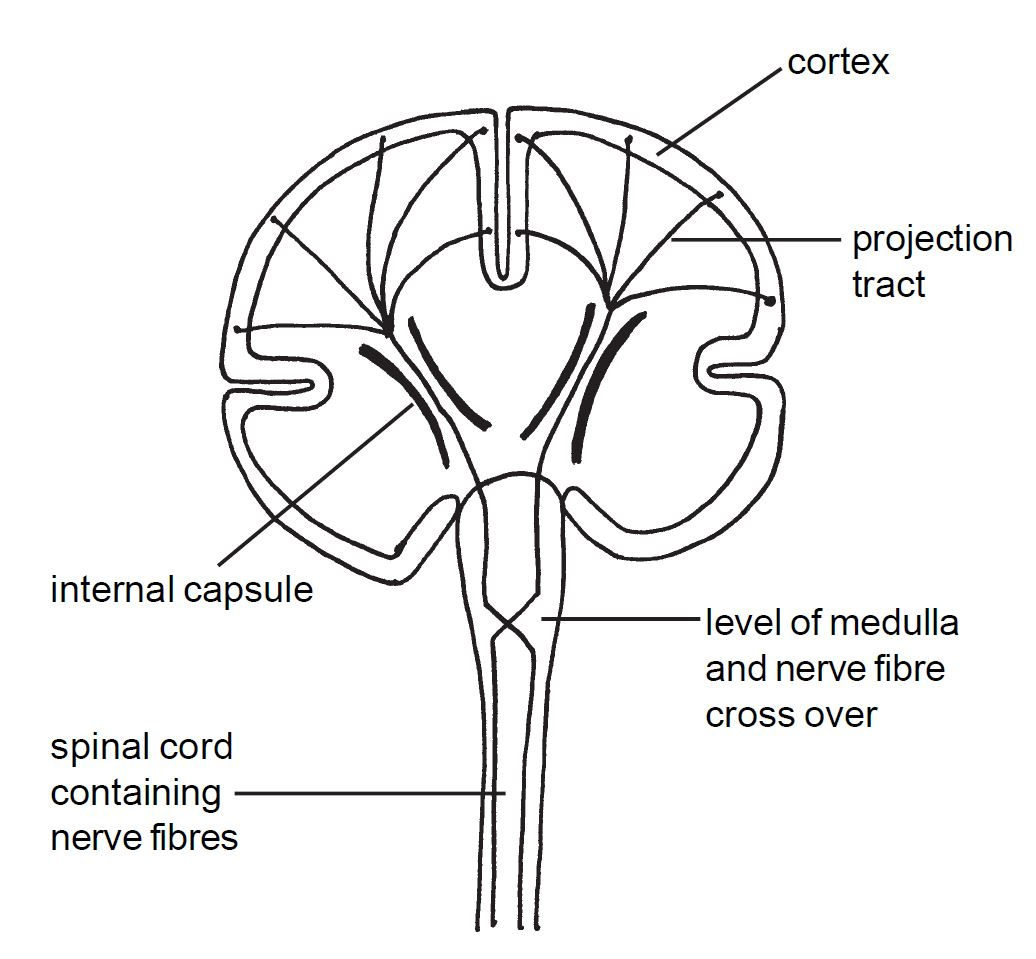
There is an internal capsule in both hemispheres of the brain. These capsules
carry nerve fibres between the cerebral cortex and brain stem. All of the motor
fibres from the motor cortex pass through this capsule. All of the sensory fibres
travelling to the sensory cortex also pass through the internal capsule.
These nerve pathways carry on through the brain stem and down the spinal
cord to the body. This means that if part of the blood supply to the internal
capsule is occluded, many nerve fibres can be infarcted which will no longer be
able to carry nerve impulses. As a result sensory information will not be able to
pass from the body to the sensory cortex and motor impulses will be unable to
pass from the cortex to the body.
Haemorrhagic pathophysiology
Haemorrhage is the other main cause of stroke. Haemorrhagic stroke caused by
intracerebral (within the cerebrum) bleeds account for about 10% of cases.
Bleeds may occur as a result of a ruptured aneurysm, which is a weakness in the
wall of a blood vessel. The explosive entry of blood into the tissues of the brain
immediately prevents the normal function of the neurones in the affected area.
The haematoma caused by the haemorrhage may be reabsorbed over time and
there may be varying degrees of patient recovery. Large bleeds may lead to raised
intracranial pressure, shifting of intracranial contents and death from coning.
In addition to cerebral haemorrhage causing stroke it is also possible for a
thromboembolic stroke to be complicated by haemorrhage. Ischaemia or
infarction caused by an arterial occlusion may damage the walls of blood vessels
as well as neurological tissue. Bleeding may then occur through this damaged
vascular wall leading to haemorrhage into the infarcted area. This is referred to
as haemorrhagic transformation.
The remaining strokes which are not thromboembolic or haemorrhagic may
be caused by cerebral hypoperfusion, subarachnoid haemorrhage and subdural
or extradural haematoma.
Aetiology and Prevention
As stroke is most commonly caused by underlying arterial disease, the risk factors
are the same as those for the development of atherosclerosis. People should be
given all of the health education advice and treatments necessary for the
prevention of atherosclerosis. In particular, hypertension is a significant risk
factor for stroke. This is important to know as high blood pressure can usually
be effectively managed, therefore reducing the risk. If heart disease is present
this should be treated as far as possible. If atrial fibrillation is an ongoing problem
then anticoagulants are important to reduce the risk of thrombi developing in
the atria.
Clinical features of stroke
There will be a sudden onset (over a few minutes) of focal neurological deficit.
Features may continue to develop over the next few hours; this is called a
stroke in evolution. Usually the clinical features reach a maximum after about
6 hours when the stroke is said to be completed.
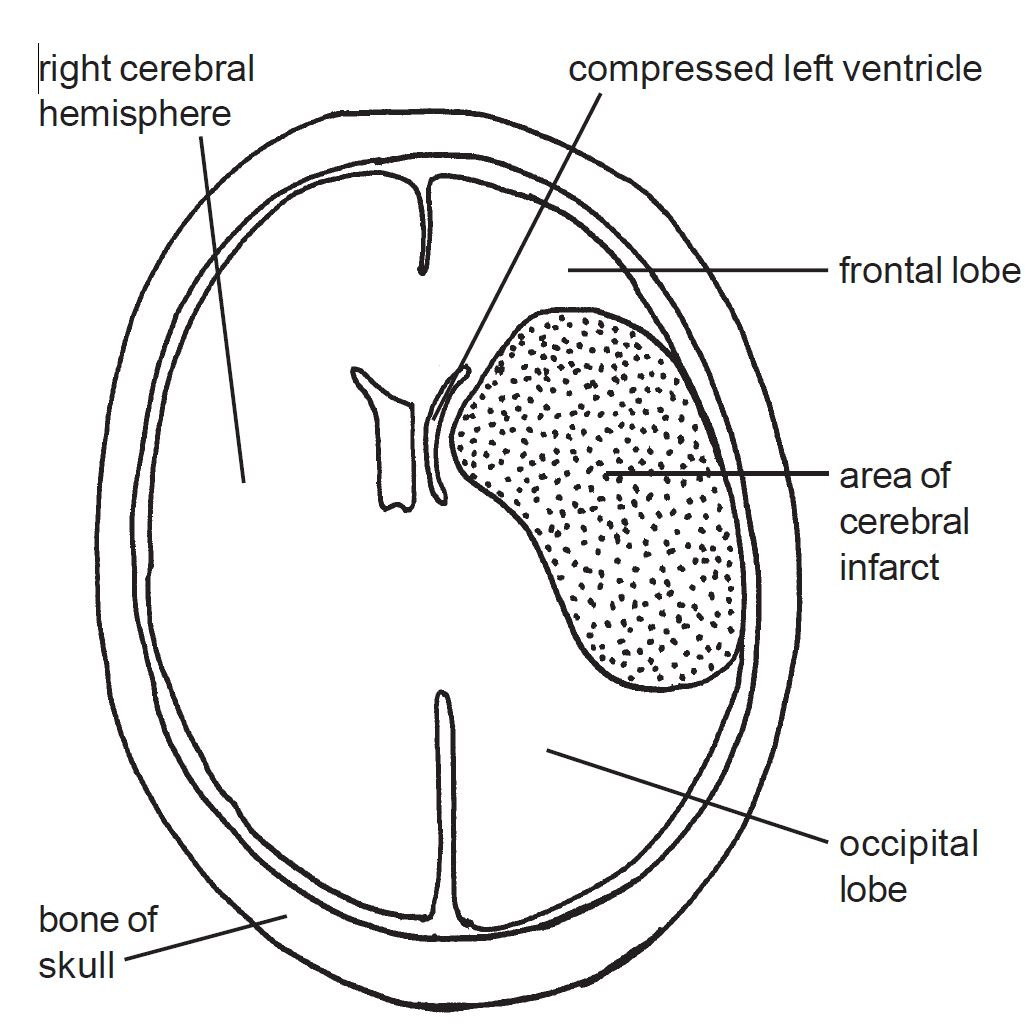
As most nerve fibres cross over at the level of the medulla oblongata, a
stroke affecting the left side of the brain will cause neurological deficit on the
right side of the body. Likewise a stroke in the right side of the brain will affect
the left side of the body. Therefore limbs on the opposite side to the cerebral
lesion become weak and may be completely paralysed. In severe cases there may
be a complete hemiplegia (paralysis of one side of the body). Other cases may
show a hemiparesis (muscular weakness on one side of the body). Often the
facial muscles on one side will be paralysed giving rise to a droop.
Sensation is also usually lost; the patient is unable to feel affected areas of
the body. Indeed the situation is often more extreme than this, patients neglect,
or even fail to acknowledge the existence of one side of the body. Some patients
may try to push their hand out of bed because they do not believe it belongs to
them.
Centres which generate speech are usually located in the dominant cerebral
hemisphere. In right handed people the dominant hemisphere is the left. This
means that if the left hemisphere is involved the speech centres may no longer
function normally. An impaired ability to generate speech is termed a dysphasia
and a complete loss of speech as aphasia. Other patients know what they want
to say but find it difficult to articulate words as a result of loss of motor function.
This feature is described as dysarthria. There may also be involvement of the
parts of the brain that facilitate the understanding of language, described as
receptive dysphasia. Dysphagia (difficulty in swallowing) is also common after
stroke. If the occipital lobes or tracts are involved there may be a sudden
deterioration of vision in one or both eyes.
Most patients remain conscious during a stroke making it a very frightening
experience. Confusion is possible but loss of consciousness usually indicates a
large lesion or the involvement of the brain stem. While severe headache and
vomiting at the onset of a stroke are possible indicators of a haemorrhagic
cause, brain imaging is needed to diagnose thromboembolic as opposed to
haemorrhagic strokes.
Prognosis
Patients have very varied recovery after a stroke. Initial recovery may be rapid
for a few days. This initial recovery can be explained by the existence of a zone
of ischaemia and inflammation around the cerebral infarction. This area of
ischaemia and inflammation, caused by the stroke, can be severe enough to
prevent normal electrical activity in the cells involved, but not severe enough to
cause them to necrose. Short term adaptations in the circulation can allow the
ischaemic area to regain an adequate level of blood perfusion and so result in a
restoration of function. If an area of brain recovers, the motor and sensory
function will be restored to the represented parts of the body. Following this
initial period, most patients show a gradual improvement and some recovery
may continue for 2-3 years. Overall about a third of patients make a good
recovery, a third are likely to die and the final third are left permanently disabled.
Management principles
Initial management must pay careful attention to maintenance of a clear airway.
Swallowing must also be assessed to prevent aspiration of saliva, food or drink
into the airway. Specialist stroke units now give thrombolysis to suitable patients
as soon as a diagnosis of thromboembolic stroke is confirmed, usually by CT
or MRI. Clearly, if a stroke has a haemorrhagic component thrombolysis would
be contraindicated. CT and MRI scanning can readily distinguish between a
haemorrhagic or thromboembolic stroke. In thromboembolic stroke aspirin
started within 48 hours has been demonstrated to improve long term outcome.
This reduces platelet aggregation and so reduces the likelihood of thrombus or
emboli formation in future. Lowering blood pressure reduces the risk of recurrent
stroke. Statins should be given to lower high plasma cholesterol and are
associated with improved outcomes. Rehabilitation is often a long process in
stroke management but can be very rewarding. Speech therapists, physiotherapists
and occupational therapists all have an important role in addition to good
nursing.
Transient ischaemic attack (TIA)
This refers to the clinical features generated by an episode of cerebral ischaemia.
Once blood flow and oxygen delivery fall below a minimum threshold neurones
will be unable to generate normal electrical activity. At this reduced level of
blood flow the neurones remain viable so infarction will not develop. Function
will recover as blood flow increases after the ischaemic episode. Traditionally a
TIA has been defined as neurological deficits which resolve within 24 hours.
The neurological deficit is caused by reduced blood flow through a partly
occluded vessel or a small thromboembolic event. While recovery is complete,
the patient should be regarded as being at risk of a future stroke.
Diagram 13.10
Sources of emboli which may enter the cerebral circulation and so lead to stroke. In atrial fibrillation there are stagnant areas of blood which may clot, mural thrombosis may complicate myocardial infarction and the arch of the aorta and carotid arteries are both common sites of atheroma formation. Emboli from extracranial vessels are the most common cause of cerebrovascular accidents. Arrows indicate the direction of emboli travel towards the brain.
Diagram 13.11
Thromboembolic stroke caused by occlusion in a large arterial
vessel. This diagram shows a large area of infarct in the left
cerebral hemisphere affecting the parietal and frontal lobes. The
cause is a thromboembolic occlusion of the middle cerebral artery.
Motor loss will occur on the right side of the body as a result of
involvement of the left motor cortex in the frontal lobe. Sensory loss
on the right side can be explained by involvement of the sensory
cortex in the left parietal lobe. It is also likely that this patient will
be aphasic as the speech centre is usually in the left hemisphere.
Diagram 13.12
From the cerebral cortex (including the motor and sensory areas) numerous fibres
pass down into the white matter of the brain. Collectively these fibres are called
the projection tracts (they are also called the corona radiata). These fibres are
all collected together in an internal capsule to be carried through the brain
to the brain stem. Most nerve fibres cross over at the level of the of the medulla
oblongata, before communicating with the body via the spinal cord.




It is disingenuous to cite long terms(in 20 years), without breaking it down by at least every five years, and when you find the five highest years, to then break it down by each year. For example: it went up 55 per ent in 20 years, but 80 percent of that rise occurred in the years 2020- 2022.
Did you want to have an open public discussion about strokes in general, or are we hinting at how mRNA induced a strokes, via clots, via endothelial damage as a result of cytotoxic T cells infiltrating and destroying mRNA transfected cells. Given Marc GIRARDOT s work clearly describing the bolus dose of mRNA in endothelium and then the subsequent and pathologically proven event whereby cd8+ killer T lymphocytes then do their fundamental job and attack (Bhakdi) obliterate (Burkhart) kill (Dr Clare) damage (Weinstein) and destroy (Campbell) the endothelial cells. This clearly triggers the coagulation pathways. Thrombosis and clots.
So these recent mRNA suddenly deaths, seizures , brain hemoraging and strokes , could be either a result of the mRNA migrating straight to the brain blood vessels, as you documented in your "brain injury" video, so that the blood brain barriwr exoresses foreing priteins and is DESTROYED by killer t lymphocytes. Resulting in localised clotting, necrosis, hemorrhaging.
Or, it could be from coagulation elsewhere in the same auto immune attack , the OBVIOUS mechanism of harm of mRNA that I have been warning of and repeating over 800,000 times over 5 years , the killer T cells attacking.
Did you want to have an open discussion about that? Who did you eat to talk to about it ? Be abuse I can talk about it for 10 hours straight, and describe how you Dr John have repeated it at least 35 times now, and in all cases, 99.999% of your audience complelty ignore you.
Or we could talk about how Dr bhakdi repeated it hundreds of times and everyone ignored him too!
Or we could talk about how I confirmed when Dr Clare Craig mentioned it in her letter to prof sexton, but when I engaged in scientific discussion, SHE was then unabke to respond .
Or we could talk about how Marc GIRARDOT has explained it and even written his book on it. And everybody says "yes, thanks, that explains the four year mystery " and the next day, 100% of people just "forget " that Marc has said anything.
Or we could discuss how now tat I have written this. With scientific. Detail. On the most important subject of our time. With pathology evidence in Dr Arne burkharts work. And validated by Marc GIRARDOT.
Then how come NOBODY will be able to have a discussion about it HERE?
Because everybody virtue signalling about truth, and stopping kids dying of mRNA, and open identifying discussion, all always seem to go silent on mass, whenever the subject of cytotoxic T cells destroying endothelium (+triggering "not -so-mysterious" clots", is mentioned.
Happy to discuss scientifically, Dr John. Offer accepted.